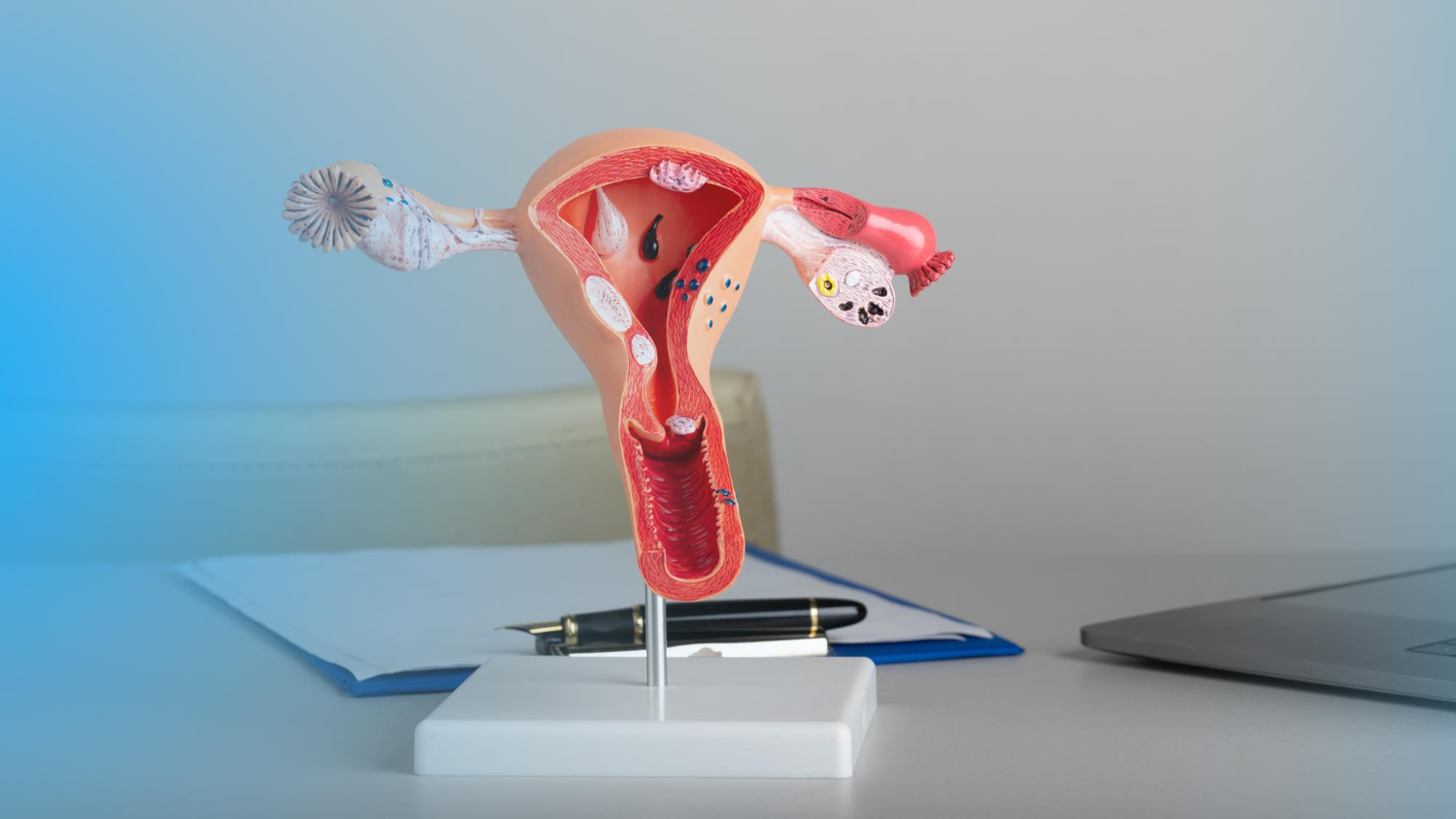
A hysteroscopy is a procedure performed by your gynaecologist to view the inside (cavity) of your uterus and cervix. This is done using a hysteroscope, a small tube-like device fitted with a camera and light at the end, which is inserted into the vagina.
There are various situations for which a hysteroscopy may be necessary. A hysteroscopy may be done to make a diagnosis or take a sample of tissue or remove a foreign body like a retained intrauterine device. Alternatively an operative hysteroscopy is done and devices are used through the hysteroscope to remove things like fibroids polyps and uterine scar tissue or septa.
Types of hysteroscopies
A diagnostic hysteroscopy
A diagnostic hysteroscopy is done to look for and confirm the diagnosis of conditions affecting the uterus or cervix. A hysteroscopy can be used in conjunction with other procedures such as laparoscopy, or before procedures such as dilation and curettage (D&C) and endometrial ablation.
Dr Guzha may dilate your cervix to allow the hysteroscope to enter the cervix and gain access to the cavity of the uterus. Fluid is then pumped into the uterus to allow for better visualisation of the uterine tissue and lining. From there, your gynaecologist will be able to examine your uterus and cervix for any abnormal lesions or growths, identifying the cause for your symptoms or abnormal pap smear results. At this time a sample is often taken using tiny instruments that are passed through the scope.
If diagnostic this procedure shouldn’t take more than 20 minutes, however, if surgery is needed small tools can be passed through the hysteroscope to perform surgery at the same time, in which case the procedure may take a bit longer.
Surgical hysteroscopy
In cases where surgery is needed to correct or treat a condition found during the diagnostic procedure then small surgical tools may be inserted into the hysteroscope to remove the given problem.
- When polyps are found, they can be treated with a procedure known as a hysteroscopic polypectomy
- When fibroids are found in the uterine cavity they can be removed. This is known as a hysteroscopic myomectomy
- When adhesions are found they can be removed surgically.
- Abnormal bleeding after menopause can be also be treated with endometrial ablation during a hysteroscopy.
- Septum than impact fertility may be removed
In the case of large fibroids in the uterine cavity the procedure may need to be repeated at serial intervals.
Hospital stay 0 – 1 days
Return to work < 1 week. For diagnostic procedures the following day.
There are risks for any procedure, but generally, a hysteroscopy is a safe procedure. The risk of complications increases with more complex cases and cases in which surgery is needed. Complications that may occur with a hysteroscopy include:
- Infection
- Fever
- Injury to the cervix.
- Perforation or injury to uterus, bowel or bladder
- Intrauterine scarring
- Heavy bleeding – resulting in the need for blood transfusion or a second operation
- Problems with your airway, breathing and heart that can be related to the anaesthesia given
These complications may require additional surgery.
You will be admitted on the day of the procedure unless otherwise indicated. After the procedure, you will be given pain medication in the ward if surgery was performed. Pain or discomfort is to be expected for the first few days, and pain medication will be prescribed. If a biopsy was taken, it might take a few weeks to get the results. Do not push anything into your vagina and refrain from sexual intercourse for 2 weeks.
If you are experiencing fever severe pain or heavy bleeding you should contact your Doctor.